One Anastomosis Gastric Bypass (OAGB)
The one anastomosis gastric bypass, also known as the Single Anastomosis Gastric Bypass (SAGB), and sometimes referred to as the mini gastric bypass, offers a unique approach to weight loss surgery.
How it works:
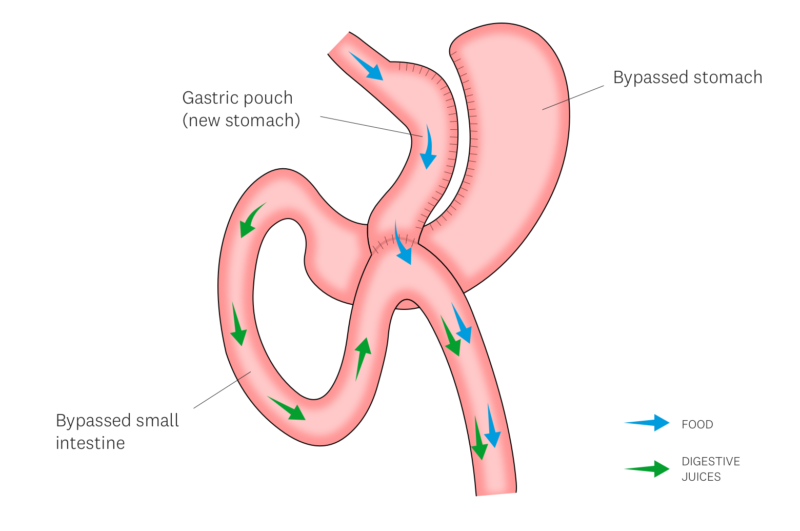
- Smaller Stomach: A portion of your stomach is reshaped into a narrow pouch, significantly reducing its volume. This limits the amount of food you can comfortably eat, leading to earlier feelings of fullness and reduced calorie intake.
- Bypassed Intestine: A section of your small intestine is rerouted, bypassing the original stomach and a portion of the small bowel. This reduces the surface area available for nutrient absorption, leading to some malabsorption of calories and nutrients.
- Minimally Invasive: The surgery is typically performed laparoscopically (keyhole approach), using several small incisions in your upper abdomen. This offers faster recovery times and less scarring compared to traditional open surgery.
Benefits:
- Combines restriction and malabsorption: Unlike the sleeve gastrectomy, the MGB offers both restriction and some malabsorption for potential faster weight loss.
- Simpler procedure: With only one connection (anastomosis) created, the MGB has a lower risk of complications compared to traditional Roux-en-Y gastric bypass surgery.
- Faster recovery: Laparoscopic surgery generally leads to quicker recovery times than open surgery.
While complications are infrequent, they can occur, and include:
- Anastomotic leak – stomach fluid may leak out into the abdomen at the join created during this procedure, due to failure of the join to heal. This may require further surgery/procedures and a prolonged hospital stay.
- Marginal ulceration – this is an erosion/ulcer of the small bowel joined to the gastric pouch, similar to a stomach ulcer. This may cause pain in the upper abdomen or chest. Most times this can be treated with medications. Occasionally, this requires revisional surgery.
- Stomal stenosis – a narrowing at the join between stomach and small bowel. You may develop vomiting and rapid weight loss, due to inability of food and/or fluids to pass through the narrowed area. This can be treated by stretching the narrowing up with a balloon, or placement of a stent (tube), and removing it 4 weeks later. Occasionally, this requires revisional surgery.
- Stomal dilation – a widening at the join between stomach and small bowel. You may feel loss of restriction and be able to eat more. This can be fixed by narrowing the opening with stitches endoscopically (via a scope placed through the mouth). Occasionally, this may require revisional surgery.
- Internal Hernia – bowel may get trapped in a space created during the formation of the gastric bypass. This may cause a blockage of the small bowel (obstruction) or lead to a lack of blood supply to the small bowel (strangulation). This is an emergency. You must go to your local hospital immediately if you have significant abdominal pain lasting more than one hour, with or without vomiting.
- Bile reflux – bile (fluid produced by the liver to help in digestion of fatty foods) may go up the oesophagus and cause symptoms similar to that of acid reflux/heartburn. This can be treated with medications. Occasionally, this may require revisional surgery.
- Dumping syndrome – a cluster of symptoms including Nausea/vomiting, rapid heartbeat, sweating, flushing, light-headedness, abdominal cramps, and diarrhoea. This is due to eating too much or eating foods high in sugar. This can be fixed by modifying your eating habits.
- Nutritional deficiencies – even though you will need to take multivitamin supplements, you can become low in certain vitamins or minerals. Additional supplementation may be necessary. You will require lifelong follow-up and blood tests to monitor for potential deficiencies.
Want to start your one anastomosis gastric bypass journey?